The Power of Community
White Paper
ABSTRACT
The evidence is compelling: organizations participating in structured innovation communities see up to 60% faster time-to-market and 40% higher implementation success rates compared to traditional development approaches.
Digital health innovation communities are transforming healthcare by creating dynamic collaborative networks that accelerate breakthrough solutions and redefine traditional business relationships. By harnessing the collective intelligence of diverse stakeholders—including health systems, payers, pharmaceutical companies, technology enterprises, and startups—these purpose-built ecosystems are dramatically shortening innovation cycles and producing solutions that no single organization could achieve alone. This paper explores how innovation communities leverage network effects to create exponential value, examines the structural elements that make them effective, and provides strategic guidance for organizations seeking to maximize their impact in this collaborative landscape.
PART 1: THE PARADIGM SHIFT IN DIGITAL HEALTH INNOVATION
This high failure rate stems from a complex interplay of healthcare-specific barriers. Innovators must navigate intricate regulatory frameworks while simultaneously addressing clinical integration requirements that vary dramatically across health systems. Meanwhile, the fundamental challenge of securing sustainable revenue persists when different stakeholders control adoption decisions and payment mechanisms.
Traditional siloed approaches to innovation simply cannot overcome these complex, interconnected challenges of modern healthcare. When "the patient is the user but not the customer," brilliant solutions fail because, despite creating tools clinicians value, they cannot secure sustainable revenue when payers don't see compelling ROI within their required timeframe.

Innovation communities represent a powerful response to this challenge—creating vibrant ecosystems where diverse expertise converges around shared healthcare problems. Unlike conventional vendor-client relationships or closed R&D approaches, these communities ignite rapid progress through frameworks of open knowledge exchange, co-creation, and shared risk. They fundamentally reimagine how digital health innovation unfolds in today's interconnected healthcare ecosystem by addressing the very barriers that typically derail promising solutions.

PART 2: THE NETWORK EFFECT— METCALF'S LAW IN HEALTHCARE INNOVATION
The extraordinary power of innovation communities can be understood through Metcalf's Law, which states that a network's value grows exponentially with each additional user. In healthcare innovation, this principle manifests dramatically as diverse stakeholders join collaborative communities.

Digital health innovation communities exemplify this principle particularly well. When clinicians, data scientists, regulatory experts, and entrepreneurs collaborate in structured environments, the resulting solutions reflect a synthesis of perspectives impossible to achieve through conventional development approaches. The key insight is that healthcare challenges are too multifaceted for any single organization to fully comprehend, much less solve in isolation.
PART 3: DIGITAL HEALTH INNOVATION COMMUNITY ECOSYSTEM: WHO BENEFITS?
The collaborative model creates distinctive value for each stakeholder group within the digital health ecosystem
0-1 YEARS
Resource Efficiency: Shared access to specialized expertise
Cost Reduction: Decreased development costs through collaboration
Network Expansion: Access to diverse healthcare stakeholders
Knowledge Acquisition: Exposure to emerging trends
Innovation communities show up to 30% reduction in development costs
1-3 YEARS
Accelerated Time-to-Market: Faster regulatory navigation
Reduced Implementation Risk: Improved design through early feedback
Enhanced Solution Quality: Better alignment with real-world needs
Partnership Development: Strategic relationships enabling broader implementation
Solutions via community approaches reach implementation 40-60% faster
3+ YEARS
Improved Clinical Outcomes: Measurable patient care improvements
Market Transformation: Disruption of established care models
System-Level Efficiency: Reduced waste across healthcare settings
Organizational Capability: Enhanced innovation capacity
Organizations in mature innovation communities report 3x higher implementation success rates
The road to ROI for Healthcare Innovation illustrates how value creation evolves over time within well-structured healthcare innovation communities. While immediate benefits justify initial participation, the transformative potential emerges through sustained engagement that drives system-level improvements in care delivery and outcomes.
HEALTH SYSTEMS
• Access to pre-vetted digital solutions addressing genuine clinical needs
• Reduced implementation risk through peer validation and shared learning
• Opportunities to shape technology development before significant investment
• Enhanced competitive positioning by accelerating digital transformation
Rather than evaluating hundreds of digital health solutions in isolation, health systems participating in innovation communities leverage collective intelligence to identify truly promising approaches, dramatically improving implementation success rates and ROI on technology investments.
PAYORS/HEALTH PLANS
Earlier visibility into emerging technologies affecting care delivery and costs
• Collaborative development of value-based care enablement tools
• Streamlined evaluation of potential reimbursement models for digital therapeutics
• Cross-organizational insights into implementation challenges and best practices
Forward-thinking payers engage in innovation communities to influence digital health development from inception, ensuring solutions align with value-based care initiatives and reimbursement capabilities—creating win-win scenarios for technology developers and payment models.
PHARMA COMPANIES
• Access to pre-vetted digital solutions addressing genuine clinical needs
• Reduced implementation risk through peer validation and shared learning
• Opportunities to shape technology development before significant investment
• Enhanced competitive positioning by accelerating digital transformation
Rather than evaluating hundreds of digital health solutions in isolation, health systems participating in innovation communities leverage collective intelligence to identify truly promising approaches, dramatically improving implementation success rates and ROI on technology investments.
ENTERPRISE TECH ORGS
• Accelerated development of digital companions for therapeutic products
• Enhanced patient engagement and medication adherence solutions
• Access to diverse real-world data for clinical development insights
• Collaborative platforms for patient-centered discovery and development
Leading pharmaceutical organizations now view digital health innovation communities as essential accelerators for developing digital therapeutics and companion tools that complement their traditional medication portfolios, enhancing both clinical outcomes and market differentiation.
DIGITAL HEALTH STARTUPS
• Critical access to clinical validation environments
• Guidance navigating regulatory pathways and reimbursement strategies
• Faster paths to adoption through established stakeholder relationships
• Capital efficiency through shared resources and accelerated development cycles
For startups facing the daunting 80% healthcare innovation failure rate, structured innovation communities provide navigational support through healthcare's complex regulatory, clinical, and reimbursement landscapes—transforming survival and success probabilities.
PART 4: UNIQUE INNOVATION ACCELERATION METHODS
The most dynamic healthcare innovation communities employ multiple mechanisms to catalyze breakthrough solutions

STRUCTURED INNOVATION CHALLENGES
Focused innovation challenges create time-bound opportunities to solve specific healthcare problems with clearly defined success criteria and implementation pathways. These challenges offer multiple benefits.
• Focus diverse expertise on narrowly defined healthcare problems
• Create healthy competition that accelerates solution development
• Provide structured paths from concept to implementation
• Generate stakeholder commitment to adopt winning approaches
Well-designed innovation challenges compress development timelines from years to months by creating constructive pressure and clear pathways from concept to implementation. For example, targeted digital health challenges around remote monitoring solutions have accelerated development cycles by over 40% compared to traditional approaches.
"SHARK TANK" STYLE COMPETITIONS
High-stakes pitch competitions with expert judging panels inject excitement while providing invaluable feedback to innovators. They serve multiple important functions in the innovation ecosystem.
• Elevate visibility for promising solutions across the ecosystem
• Provide constructive critique from diverse stakeholder perspectives
• Create networking opportunities between innovators and implementation partners
• Build entrepreneurial capabilities within participating organizations
These high-visibility events create compelling platforms for solution evaluation while developing presentation and commercialization skills across the ecosystem. More importantly, they establish clear implementation pathways for winning approaches, avoiding the "pilot purgatory" that strands many digital health innovations.
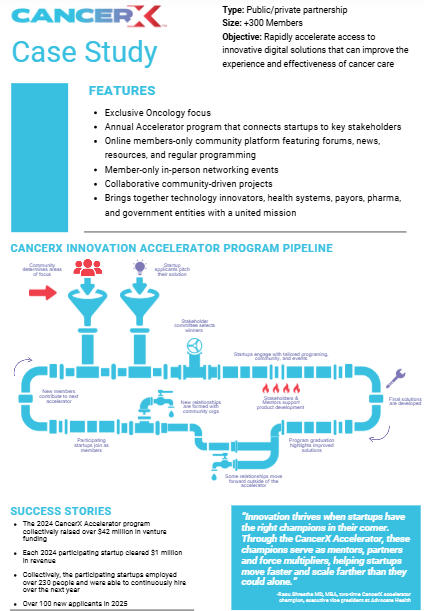
COLLABORATIVE ACCELERATOR PROGRAMS
Specialized accelerator programs nurture promising solutions through critical development stages with mentorship from across the ecosystem:
• Provide structured business development guidance from industry experts
• Create cohort-based peer learning environments
• Facilitate connections to potential customers, partners and investors
• Accelerate regulatory strategy development and market entry planning
Unlike traditional accelerators focused primarily on investment readiness, community-based healthcare accelerators emphasize implementation pathways and clinical validation—addressing the integration challenges that frequently derail promising digital health innovations after initial funding.
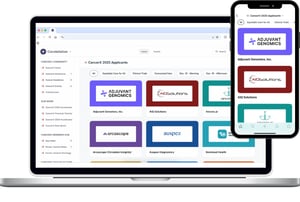
OPEN INNOVATION PLATFORMS
Digital platforms facilitate continuous collaboration beyond time-bound events. Through these platforms, organizations can achieve several ongoing collaboration objectives.
• Enable asynchronous idea sharing and problem solving
• Document collective knowledge and insights for future reference
• Support matchmaking between complementary capabilities
• Facilitate governance and intellectual property management
These always-on collaboration infrastructures overcome the geographic and organizational boundaries that typically constrain healthcare innovation, creating persistent environments where insights and relationships develop organically between formal initiatives.
PART 5: THE ARCHITECTURE OF SUCCESSFUL DIGITAL HEALTH INNOVATION COMMUNITIES
Effective digital health innovation communities require thoughtfully designed structural elements that balance flexibility with sufficient structure to drive outcomes
The landscape of digital health innovation is increasingly defined by collaborative ecosystems rather than isolated actors. This section examines the architectural elements that distinguish high-performing innovation communities in healthcare from their less effective counterparts. Drawing on research from successful implementations, we explore four foundational pillars: governance models that balance structure with autonomy, strategic approaches to stakeholder diversity, specialized knowledge exchange infrastructure, and multidimensional value measurement frameworks. Together, these elements create the conditions where breakthrough healthcare solutions can emerge through structured collaboration while addressing the unique regulatory, clinical, and technical complexities inherent to the healthcare domain.
GOVERNANCE MODELS THAT BALANCE STRUCTURE WITH AUTONOMY
The most successful communities establish clear frameworks while preserving space for emergent collaboration. Effective governance typically includes several key elements.
• Decentralized decision-making that empowers participants
• Transparent processes for setting priorities and allocating resources
• Clear intellectual property frameworks that encourage sharing while protecting key interests
• Adaptive governance that evolves as the community matures
Research into successful healthcare innovation communities reveals that governance effectiveness follows a "Goldilocks principle"—too little structure yields unfocused activity, while excessive rigidity stifles the creative collaboration essential for breakthrough solutions. The most productive models employ polycentric governance that balances clear frameworks with participant autonomy.
DIVERSE STAKEHOLDER ENGAGEMENT STRATEGIES
Vibrant communities actively cultivate participation across the healthcare ecosystem. Many successful innovation networks employ the following approaches.
• Clinical voices integrated throughout the innovation process
• Cross-sector representation in leadership and working groups
• Deliberate inclusion of complementary capabilities and perspectives
• Balanced participation from organizations of different sizes and maturity levels
Strategic diversity is the cornerstone of effective innovation communities. Leading healthcare innovation networks deliberately engineer stakeholder composition to ensure complementary perspectives across the care delivery, payment, technology, and regulatory domains—creating comprehensive solution environments.
KNOWLEDGE EXCHANGE INFRASTRUCTURE
Purpose-built systems facilitate information sharing while respecting healthcare's unique constraints. Successful infrastructures often incorporate several specialized components.
• Secure collaboration platforms with healthcare-specific privacy safeguards
• Structured knowledge management systems that capture and disseminate insights
• Clinical resource-sharing mechanisms (data commons, testing environments, etc.)
• Translation services that bridge technical and clinical language barriers
Successful digital health innovation communities develop specialized knowledge exchange mechanisms that address domain-specific challenges, including health data privacy regulations, clinical workflow integration requirements, and evidence-based validation standards. These purpose-built infrastructures enable secure knowledge flow while maintaining essential trust.
VALUE CREATION AND MEASUREMENT FRAMEWORKS
Successful communities clearly articulate and measure the benefits they create. Leading organizations implement multiple measurement approaches to capture impact.
• Balanced metrics encompassing both tangible outputs and relationship development
• Attribution models that recognize diverse contributions to innovation
• Longitudinal tracking that captures both short-term wins and system-level impacts
• Transparent reporting that demonstrates value to all stakeholder groups
Research confirms that effective innovation communities employ mixed-methods evaluation approaches that balance quantitative metrics with qualitative insights. This multidimensional measurement approach captures both immediate outputs and longer-term capability development, essential for demonstrating holistic ROI to participating organizations.
PART 6: BUILD, BUY, OR BLEND? STRATEGIC APPROACHES FOR NEW COMMUNITIES
Healthcare organizations face important strategic choices in how they engage with innovation communities

Healthcare organizations face a pivotal strategic question: should they build their own innovation communities, partner with established orchestrators, or pursue a blended approach? This section examines the critical decision frameworks, resource considerations, and strategic implications of different community engagement models. By carefully evaluating organizational capabilities, innovation objectives, and market positioning, healthcare leaders can develop community strategies that accelerate innovation while optimizing resource allocation and competitive advantage.
BUILD VS PARNTER DECISION FRAMEWORK
Organizations must thoughtfully assess whether to create their own communities or join existing ones. This assessment should evaluate several critical factors.
• Strategic alignment with organizational priorities and capabilities
• Resource requirements for different community engagement models
• Timeline considerations for achieving innovation objectives
• Competitive positioning and differentiation opportunities
The build-versus-partner decision should be guided by organizational capabilities, resources, and strategic objectives. Building proprietary innovation communities offers greater control but requires substantial investment in platform development, staffing, and operations. Partnering with established orchestrators provides faster time-to-value with reduced capital expenditure, though with less control over community direction.
HYBRID APPROACHES FOR MAXIMUM IMPACT
Many organizations benefit from combined strategies that leverage different community models. Common hybrid approaches include the following methods.
• Participation in broad ecosystem communities for general insights and relationships
• Focused micro-communities addressing specific organizational priorities
• Staged evolution from partnership to leadership as capabilities develop
• Complementary investments in internal and external innovation capabilities
Healthcare organizations increasingly adopt hybrid approaches that combine elements of both build and buy strategies to gain maximum advantage. Many find success by initially partnering with established orchestrators to launch their innovation communities while simultaneously developing internal capabilities for eventual self-management. Others create specialized subcommunities within larger established innovation networks, allowing them to focus on specific clinical areas while benefiting from the broader ecosystem's resources and connections.

CONCLUSION
The challenges facing healthcare—from chronic disease management to health equity to workforce shortages—are simply too complex for any single organization to solve alone. Innovation communities represent our most promising path forward, creating environments where breakthrough solutions can emerge from the collective intelligence of the entire healthcare ecosystem.
The evidence is compelling: organizations that engage strategically in well-designed innovation communities see measurably faster development cycles, higher implementation success rates, and greater market impact than those following traditional siloed approaches. In an ecosystem where 98% of digital health startups struggle despite promising technologies, structured innovation communities provide the critical translational infrastructure that bridges the chasm between great ideas and implemented solutions.
For forward-thinking healthcare leaders, the strategic imperative is clear: active participation in well-designed innovation communities is no longer optional but essential for organizational relevance and impact. The organizations that thrive in tomorrow's healthcare landscape will be those that most effectively harness the exponential power of community-driven innovation—transforming not just their own capabilities but contributing to a fundamentally more collaborative and effective healthcare system for all.
The future of Digital Health innovation is community-driven.
Accelerate your healthcare innovation today.
Contact Decimal Health to drive decisive results and conquer market challenges with precision.
SOURCES
- Agri India Today. (2025, January). Environmental Services Market in India. https://agriindiatoday.in/Volume-05-Issue-01-January-2025.pdf
- CET Partnership. (2025). Energy Industry in Europe. https://cetpartnership.eu/sites/default/files/documentation/CETPartnership%20Joint%20Call%202023%20Call%20Text_approved_v2023-09-28.pdf
- European Investment Fund. (2025). EIT health skills European health sector. http://www.eif.org/news_centre/publications/eithealth-skills-european-health-sector.pdf
- European Union Council. (2025). Advanced IT Market in the EU. https://eurocid.mne.gov.pt/sites/default/files/repository/paragraph/documents/11576/investeufinalreportclean.pdf
- European Patent Office. (2025). Mapping investors for European innovators. https://link.epo.org/web/publications/studies/en-mapping-investors-for-european-innovators.pdf
- European Startup Network Alliance. (2025). Artificial Intelligence Market in the EU. https://www.esnalliance.eu/multimedia/esna/esna-compendium-1.pdf
- Health Tech World. (2022, December 28). The top 3 reasons health tech startups fail. https://www.htworld.co.uk/news/the-top-3-reasons-health-tech-startups-fail/
- Henry Royce Institute. (2025, January). National Materials Innovation strategy. https://www.royce.ac.uk/content/uploads/2025/01/National_Materials_Innovation_Strategy_FINAL_WEBSITE.pdf
- International Energy Agency. (2025). The state of energy innovation. https://iea.blob.core.windows.net/assets/26e9f71e-3a3f-4c82-802b-c2ed97aaae24/Thestateofenergyinnovation.pdf
- L-Camp EU. (2023, July). Manufacturing Industry Trends in Europe. https://lcamp.eu/wp-content/uploads/sites/53/2023/07/D3.2-Observatory_reportN1-2.pdf
- Legacy of Game. (2025). White paper. https://www.legacyofgame.io/white-paper.pdf
- LEK Consulting. (2025). APAC medtech innovation engine. https://www.lek.com/sites/default/files/PDFs/APAC-medtech-innovation-engine.pdf
- Masternoder. (2025). Global Cryptocurrency Market. https://masternoder.dk/PDF/MN2%20report.pdf
- Middle East University. (2025). E-Services economic impact in Turkey. https://open.metu.edu.tr/bitstream/handle/11511/112709/0009-0003-4400-3326.pdf
- PMC. (2024). What is coming next in health technology startups? Some insights and practice guidelines. https://pmc.ncbi.nlm.nih.gov/articles/PMC10668566/
- Revli. (2024). 50 Must-know startup failure statistics in 2024. https://www.revli.com/blog/50-must-know-startup-failure-statistics-2024/
- STAT. (2022, September 13). 10 reasons why health care startups fail. https://www.statnews.com/2020/02/10/10-reasons-why-health-care-startups-fail/
- Surrey City. (2024, February). Real Estate Economic Impact in Canada. https://www.surrey.ca/sites/default/files/media/documents/DCT_Closed_Resolution_2024_02_15.pdf
- Syscreations. (2024, September 30). 97% of health tech startups fail: 3 basic mistakes they make. https://www.syscreations.com/digital-health-tech-startups/
- Tecco, H. (2024, June 26). Why healthcare startups fail. https://www.halletecco.com/blog/why-healthcare-startups-fail
- World Energy Council. (2025, March). Issues monitor 2025 full report. http://wec-chile.cl/wp-content/uploads/2025/03/Issues_Monitor_2025_Full_report_FINAL.pdf Council. (2025, March). Issues monitor 2025 full report. http://wec-chile.cl/wp-content/uploads/2025/03/Issues_Monitor_2025_Full_report_FINAL.pdf
.png?width=125&height=125&name=logo_wt%20(3).png)





.png?width=300&name=CancerX%20Decimal%20Banner%20(2).png)