
Is "Care at Home" the Future?
White Paper
ABSTRACT
The shift toward home-based healthcare offers tremendous advantages, with approximately 15-20% of emergency and urgent care services and 30-35% of hospice care already suitable for in-home delivery.
This white paper examines the resurgence of Care at Home (CaH) in the healthcare industry, a practice that was common in the 1930s but later became obsolete due to scalability and reimbursement challenges. The COVID-19 pandemic served as a catalyst for this revival, enabling widespread implementation of home-based care models through initiatives like the Acute Hospital Care at Home program. Through analysis of current trends, case studies, and market projections, we demonstrate that CaH has moved beyond a temporary pandemic response to become a sustainable healthcare delivery model. The paper explores how technological innovations, evolving payment structures, supportive legislation, and patient preferences are driving adoption across the healthcare landscape. While highlighting the clinical and operational successes of organizations that have implemented various CaH models, we also address the challenges that must be overcome for widespread adoption. This analysis supports the conclusion that CaH represents a significant transformation in healthcare delivery that is positioned to become a standard component of modern healthcare systems.
PART 1: THE HISTORY OF CaH
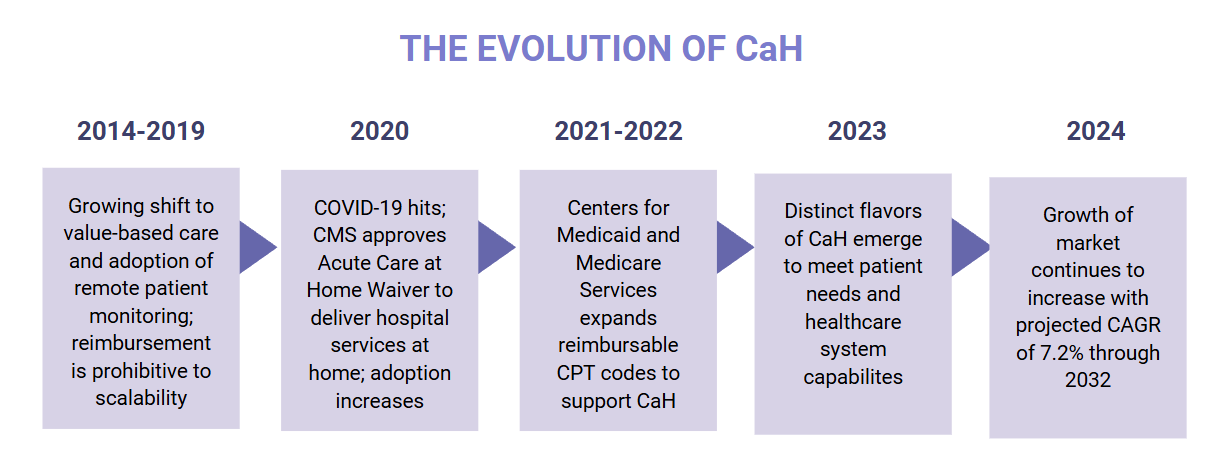
The history of healthcare delivery has often alternated between institutional and home settings. In the 1930s, approximately 40% of healthcare services were delivered in patients' homes, a practice that subsequently declined as hospital-based care became the standard model. This shift away from home-based care was primarily driven by limitations in scalability and inadequate reimbursement structures. However, modern technological innovations and evolving payment methodologies have created a foundation for the revival of home-based care delivery.
The COVID-19 pandemic proved to be a defining moment for Care at Home (CaH), as it necessitated alternatives to traditional facility-based care. The implementation of the Acute Hospital Care at Home (ACAH) initiative represented a significant policy response, allowing Medicare-certified hospitals to provide inpatient-level care in patients' homes. By April 2024, this program had expanded dramatically, with over 320 hospitals across 133 health systems in 37 states offering such services. This rapid adoption demonstrated not only the feasibility of CaH models but also their potential to transform healthcare delivery beyond the pandemic response.
The continued momentum behind CaH in the post-pandemic landscape indicates a fundamental shift in how healthcare services are conceptualized and delivered. This white paper explores the factors driving this transformation, examines successful implementation models, and addresses the challenges that must be overcome for CaH to achieve its full potential as a standard component of modern healthcare systems.
PART 2: UNDERSTANDING CaH
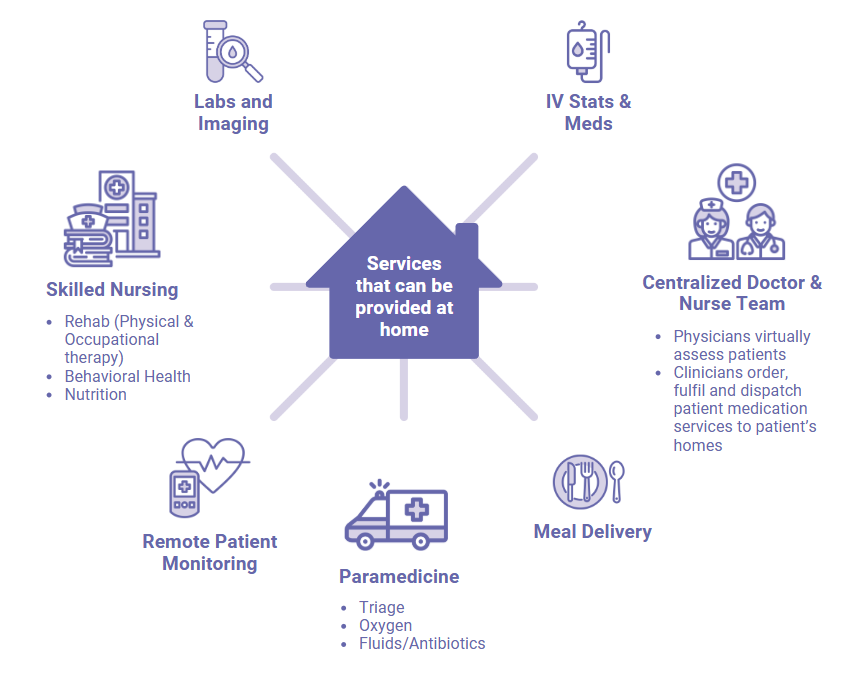
Care at Home encompasses a wide range of healthcare services delivered in patients' homes rather than in traditional healthcare facilities. In a comprehensive CaH model, patients maintain connections with their care teams through a combination of in-person visits, telehealth consultations, and continuous remote monitoring. The services provided can span the spectrum from diagnostic studies to complex treatments such as intravenous medications and oxygen therapy, as well as specialized services including respiratory therapy and skilled nursing care.
What distinguishes modern CaH from historical home-based care is the integration of technology and the development of standardized protocols that ensure consistent, high-quality care. Remote patient monitoring devices collect vital signs and other biometric data, which are transmitted to healthcare providers for real-time analysis. This continuous flow of information allows for proactive interventions and adjustments to treatment plans, creating a dynamic care environment that can respond rapidly to changes in patient status.
The traction gained by CaH models stems from their ability to deliver outcomes comparable to traditional inpatient care while offering distinct advantages. Healthcare organizations have found that these models can generate additional revenue streams by treating more patients within existing resources. By transferring appropriate patients to home-based care settings, hospitals can make inpatient beds available for higher-acuity patients who require the intensive resources of a hospital environment. This optimization of resources addresses capacity challenges while maintaining or improving the quality of care.
From the patient perspective, receiving care at home reduces the disruption associated with hospitalization and minimizes exposure to healthcare-associated infections. The familiar environment often contributes to improved psychological well-being and may facilitate faster recovery. These benefits align with broader healthcare goals of enhancing patient experience while reducing costs and improving outcomes.
WHY ARE HOSPITALS EMBRACING CaH?
Hospitals across the healthcare landscape are increasingly embracing care-at-home models as a strategic response to evolving patient preferences and healthcare economics. This shift is being driven by advances in remote monitoring technology, growing evidence of comparable clinical outcomes, and the pressing need to reduce facility overcrowding while managing costs. Care-at-home programs allow hospitals to extend their reach beyond traditional walls, creating virtual capacity without capital-intensive construction, while offering patients the comfort, convenience, and familiarity of their home environment. As healthcare systems face ongoing capacity constraints and staffing challenges, this model represents not just an alternative care setting but an essential component of the modern healthcare delivery ecosystem.

PART 3: ADOPTION AND SUCCESS MODELS
The fundamental components of successful home-based care models demonstrate measurable outcomes in both patient satisfaction and operational efficiency through their thoughtful implementation across diverse healthcare contexts.
CaH MODEL BASICS
In a Care at Home (CaH) model, patients connect with healthcare providers through a blend of in-person visits, virtual consultations, and remote monitoring. Services delivered at home include diagnostics, treatments like oxygen therapy and IV medications, and clinical support such as respiratory therapy and skilled nursing. Care team members work collaboratively, following individualized care plans and evidence-based protocols to adjust care intensity based on patient needs. This approach transforms homes into clinical settings that maintain hospital-level oversight while offering patients the comfort and psychological benefits of healing in familiar surroundings.
THE MAYO EXAMPLE
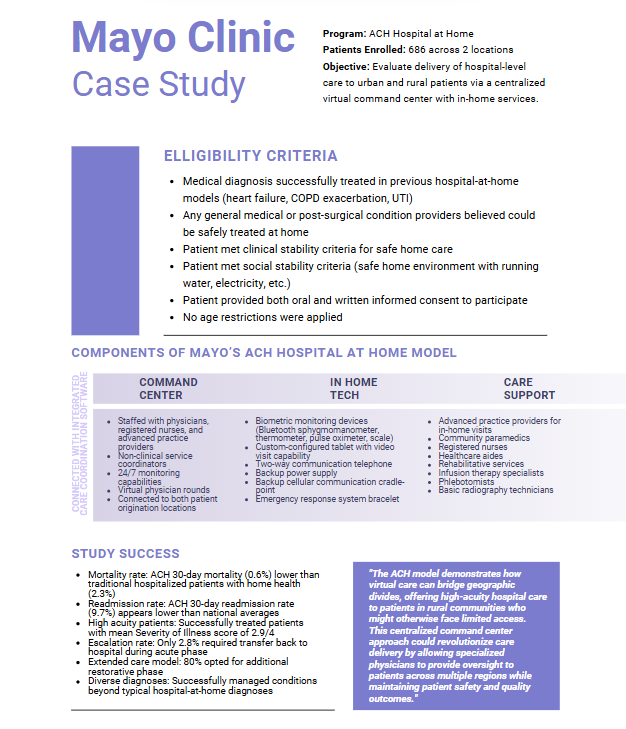
The experience of Mayo Clinic provides a compelling case study of successful CaH implementation. Mayo's hospital-at-home program has treated nearly 700 patients distributed across locations separated by 1,000 miles. With 408 patients enrolled in Jacksonville, Florida, and 278 in Eau Claire, Wisconsin, the program has achieved clinical outcomes comparable to traditional inpatient care while demonstrating significant operational efficiencies.
At the heart of Mayo's success is its virtual command center, which enables 20 doctors and nurses to simultaneously care for up to 150 patients. This staffing efficiency stands in stark contrast to traditional models—a nearby hospital facility that is 20 times larger requires eight times more staff but can only treat twice as many patients. This comparison highlights the potential for CaH models to address healthcare workforce challenges while maintaining high standards of care.
The Mayo Clinic example illustrates how healthcare systems can optimize resource utilization through technological innovation and process redesign. By centralizing monitoring and coordination functions, clinicians can focus their attention on patients who require the most intervention while maintaining oversight of those with more stable conditions. This approach not only enhances operational efficiency but also allows for more personalized care tailored to individual patient needs.
Other healthcare organizations have developed variations of the CaH model to address specific needs within their patient populations and operational contexts. These adaptations demonstrate the flexibility of the CaH concept and its capacity to evolve in response to local requirements and constraints. The common thread across these implementations is the commitment to delivering high-quality care in settings that maximize patient comfort and minimize unnecessary resource utilization.
PART 4: POLICY AND PAYMENT EVOLUTION
After COVID-19, the momentum behind CaH remained strong as hospitals were able to establish similar clinical outcomes as inpatient care and maintain reimbursement levels.
The sustainability of CaH models depends heavily on supportive policy frameworks and appropriate reimbursement mechanisms. Recognizing this dependency, more than 65 healthcare organizations, primarily hospital systems including Kaiser Permanente, Mayo Clinic, and Johns Hopkins Medicine, have advocated for making the ACAH program permanent. This collective action reflects the growing consensus within the healthcare community regarding the value of home-based care models.

Legislative progress has been significant. In May 2024, the introduction of the 'Hospital Inpatient Services Modernization Act of 2024' proposed a five-year extension of the ACAH waiver through 2029. Additionally, federal telehealth waivers have been extended until 2026, maintaining provisions that enable home-based care delivery without geographic restrictions and including allowances for audio-only consultations. These extensions provide crucial stability for organizations investing in CaH infrastructure and capabilities.
Parallel developments in reimbursement structures have further strengthened the financial foundation for CaH. The Centers for Medicare & Medicaid Services (CMS) has introduced five new codes for remote therapeutic monitoring (RTM) that allow hospitals to bill separately for various monitoring and management services. This expansion of billable services increases the financial viability of home-based care programs and encourages their adoption by healthcare providers.
The alignment of CaH with value-based care initiatives represents another significant policy development. Models such as the Home Health Value-Based Purchasing (HHVBP) program provide financial incentives for home health agencies that demonstrate improvements in quality metrics. As healthcare financing continues to shift from volume-based to value-based approaches, CaH models that deliver high-quality outcomes with efficient resource utilization are likely to receive increasingly favorable reimbursement.
PART 4: THE EXPANDING CaH LANDSCAPE
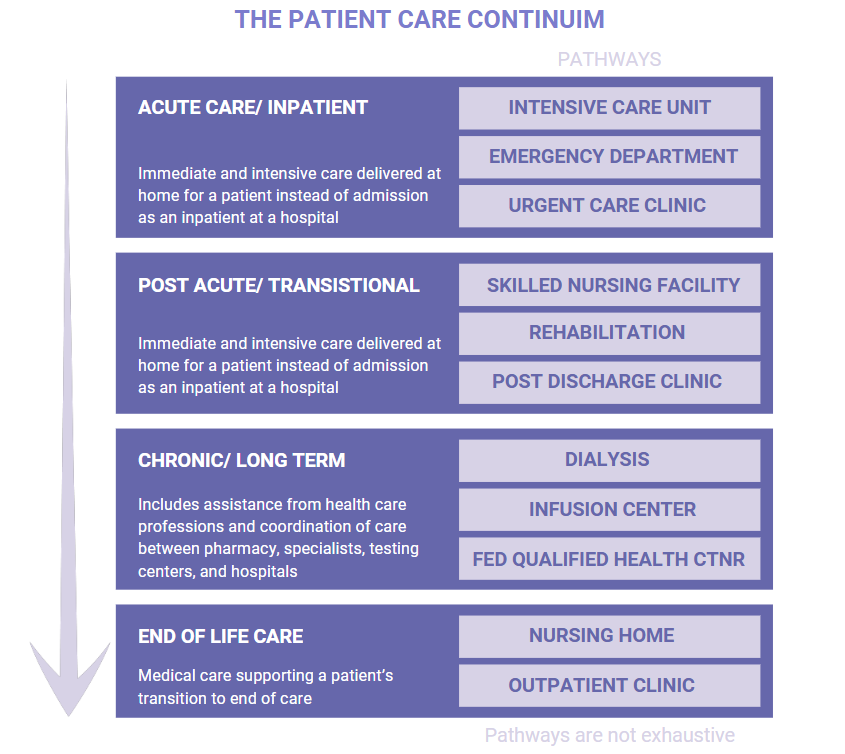
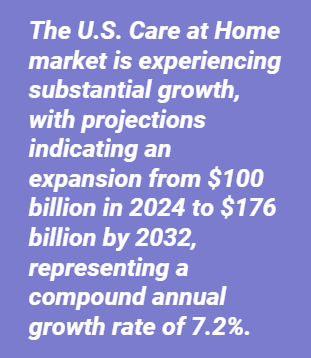
CaH growth reflects the disruption occurring across the entire care continuum—from acute care to post-acute, long-term, and palliative care—as services traditionally provided in institutional settings increasingly shift to home-based delivery.
The evolution of CaH has generated a diverse array of models tailored to specific patient populations and clinical needs. Patients now enter CaH programs through multiple pathways: directly from urgent care, through early discharge from hospital stays, or as an alternative to skilled nursing facility placement. Each entry point has led to the development of specialized approaches that maintain the core principles of CaH while addressing the unique requirements of different clinical scenarios.
The strategic partnership between Emory Healthcare and DispatchHealth represents just one example of the groundbreaking collaborative models developing in the home-based care ecosystem. Their partnership emphasizes two distinct models: Urgent Care at Home and ED to Home. Under the Urgent Care at Home model, patients can request emergency care-trained medical teams equipped with diagnostic and treatment capabilities equivalent to urgent care facilities. These teams are prepared to address a range of conditions including injuries, COPD exacerbations, and congestive heart failure, bringing acute care services directly to patients' doorsteps.
The ED to Home model targets patients at high risk of hospital readmission, aiming to reduce emergency department overcrowding while providing comprehensive care. The services offered include thorough physical examinations, medication reconciliation, health literacy evaluations, and attention to social determinants of health. The teams can perform various interventions including point-of-care laboratory tests, medication administration, intravenous fluid therapy, wound care, and catheter management. By spending 30-45 minutes with each patient and maintaining communication with primary care providers, these teams ensure continuity of care and smooth transitions between care settings.
As noted by Will ElLaissi, MD of innovation at Emory Healthcare, "ED to Home program allows us to reduce the length of time a patient is staying in a hospital when lower-touch, lower-cost settings would provide just as much benefit." This perspective captures the essence of CaH's value proposition: delivering appropriate care in the most efficient setting without compromising quality or patient experience.
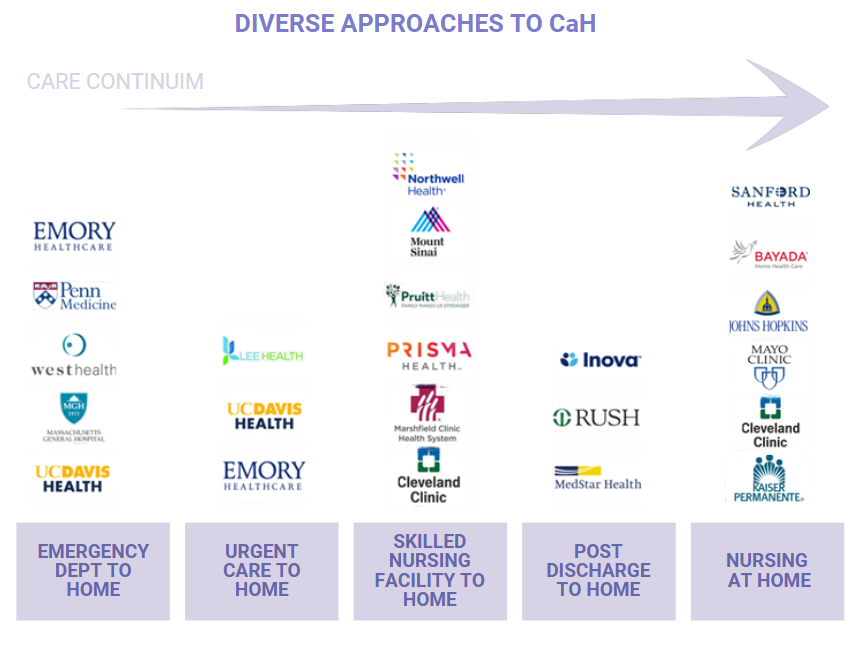
Healthcare organizations have developed several distinct Care at Home models to address specific patient needs across the care continuum. As shown above, these approaches include ED to Home services that prevent unnecessary hospitalizations, Urgent Care at Home that brings emergency-trained teams to patients' residences, SNF to Home programs that replace facility-based post-acute care, Post-Discharge services focused on preventing readmissions, and Nursing at Home for skilled care delivery. Leading health systems like Mayo Clinic, Emory Healthcare, and Kaiser Permanente have strategically implemented these models based on their organizational strengths and patient populations, demonstrating how the Care at Home concept can be tailored to diverse clinical scenarios while maintaining high-quality, patient-centered care.
PATIENT EXPERIENCE AND DEMOGRAPHICS
The patient-centered nature of CaH represents one of its most compelling advantages. Patients often express preference for receiving care in familiar environments, where they can maintain their routines and connections with family members. This comfort can contribute to improved psychological well-being, which may accelerate recovery and enhance overall health outcomes.
Beyond the psychological benefits, CaH offers practical advantages for patients. By remaining at home, individuals avoid the inherent risks associated with hospitalization, particularly healthcare- associated infections that affect a significant percentage of hospitalized patients annually. For individuals with disabilities or chronic conditions, home-based care eliminates the challenges of transportation to healthcare facilities and navigating complex institutional environments.
Demographic trends suggest that demand for CaH services will continue to grow. The U.S. Census Bureau projects that individuals aged 65 and older will comprise more than 20% of the population by 2030. This demographic shift will increase demand for healthcare services that address the complex needs of older adults, many of whom have multiple chronic conditions requiring ongoing management. CaH models are particularly well-suited to meet these needs through continuous monitoring and regular interventions that can prevent acute exacerbations and reduce the need for emergency care.
The alignment between patient preferences and demographic trends creates a strong foundation for the continued expansion of CaH. As healthcare consumers become increasingly informed and empowered in their healthcare decisions, the demand for models that prioritize convenience, comfort, and personalization is likely to accelerate. Healthcare organizations that respond to these preferences with well-designed CaH programs will gain competitive advantages in increasingly consumer-driven healthcare markets.
70% of adults feel comfortable with in-home care, 73% trust its quality, and 85% would recommend it. -Moving Health Home Survey
IMPLEMENTATION REALITIES
Despite the significant progress and potential benefits of CaH, several challenges must be addressed for these models to achieve widespread adoption and sustainable impact. Financial sustainability remains a primary concern for many healthcare organizations considering CaH implementation. Developing programs that generate positive returns on investment requires careful attention to payment pathways and cost optimization.

The current landscape of fee-for-service and diagnosis-related group reimbursement provides limited incentives for hospitals to develop comprehensive CaH programs. While value-based payment models are increasingly supportive of home-based care, the transition from volume-based to value-based financing remains incomplete. Organizations must navigate this complex payment environment while building financially sustainable models that can survive in mixed reimbursement contexts.
Technology represents both an enabler and a challenge for CaH implementation. The effective delivery of home-based care depends on reliable remote monitoring systems, secure communication platforms, and integrated data management solutions. Developing and maintaining this technological infrastructure requires significant investment and ongoing attention to evolving capabilities and requirements. Organizations must carefully evaluate their technological readiness and develop strategic plans for acquiring and implementing the necessary tools and systems.
Operational challenges also influence CaH implementation. Developing comprehensive strategies that address logistical constraints, workforce requirements, and governance structures is essential for integrating CaH into mainstream healthcare practices. Organizations must establish clear protocols for patient selection, care delivery, monitoring, and escalation of care when necessary. These protocols must ensure consistency across care teams while allowing for appropriate personalization based on individual patient needs.
As Dr. Kamal Jethwani, CEO of Decimal Health, observes:
"Care at Home is poised to become a permanent fixture in healthcare due to its demonstrated positive outcomes across hospitals, payers, and patients and the technological, and regulatory trends that make it possible."
However, realizing this potential requires acknowledging and addressing the financial, technological, and operational challenges that currently limit CaH adoption and impact.
CONCLUSION
Care at Home has emerged from the COVID-19 pandemic as a viable, sustainable approach to healthcare delivery that offers benefits to patients, providers, and healthcare systems. The evidence presented in this white paper demonstrates that CaH has moved beyond a temporary pandemic response to become a significant component of the healthcare landscape with substantial growth potential.
The success of organizations like Mayo Clinic in implementing hospital-at-home programs illustrates the clinical and operational viability of these models. By achieving outcomes comparable to traditional inpatient care while optimizing resource utilization, these programs demonstrate that quality and efficiency can be enhanced simultaneously through well-designed home-based care delivery.
The evolving policy and payment environment increasingly supports CaH implementation. Legislative extensions of telehealth and hospital-at-home waivers provide stability for organizations investing in these capabilities, while new reimbursement codes improve the financial sustainability of home-based care programs. The alignment between CaH and value-based care initiatives creates a foundation for continued expansion as healthcare financing increasingly rewards quality and efficiency.
For CaH to fully achieve its potential, healthcare organizations must address challenges related to financial sustainability, technological requirements, and implementation strategies. By developing ROI-positive programs, leveraging appropriate technologies, and implementing effective operational models, organizations can overcome these challenges and establish CaH as a standard component of modern healthcare delivery.
The future of healthcare will feature a blend of facility-based and home-based care, with services delivered in the setting that best meets individual patient needs while optimizing resource utilization.
Care at Home is not merely a pandemic adaptation—
it represents a fundamental transformation in healthcare delivery that brings the power of the hospital to the healing environment of home.
Accelerate your healthcare innovation today.
Contact Decimal Health to drive decisive results and conquer market challenges with precision.
SOURCES
- (2024). bill. HR 4040.
- (2024). bill. S-3792.
- Amedisys. (2022, June 9). Baylor Scott & White Health and Contessa announce partnership to create new model of at-home care for patients. Amedisys Inc. https://investors.amedisys.com/news/news-details/2022/Baylor-Scott--White-Health-and-Contessa-Announce-Partnership-to-Create-New-Model-of-At-Home-Care-for-Patients/default.aspx
- Bayada. (2025). Bayada home health care services – the highest-level care in the comfort of home. Red text BAYADA 50 years. https://www.bayada.com/services
- Bestsennyy, O., Chmielewski, M., Koffel, A., & Shah, A. (2022, February 1). From facility to Home: How Healthcare could shift by 2025. McKinsey & Company. https://www.mckinsey.com/industries/healthcare/our-insights/from-facility-to-home-how-healthcare-could-shift-by-2025
- Clabaugh, J. (2024, April 15). MedStar health teams with DispatchHealth for in-home hospital stay follow-ups. WTOP News. https://wtop.com/business-finance/2024/04/medstar-health-teams-with-dispatchhealth-for-in-home-hospital-stay-follow-ups/
- Cleveland Clinic. (2025). Home care. https://my.clevelandclinic.org/departments/connected-care/services/home-care
- CMS.gov. (2024, September 30). Fact sheet: Report on the study of the Acute Hospital Care at Home initiative. https://www.cms.gov/newsroom/fact-sheets/fact-sheet-report-study-acute-hospital-care-home-initiative
- Connolly, L. (2024a, November 27). “The Next Frontier of Emergency Medicine”: House calls following emergency room. news. https://health.ucdavis.edu/news/headlines/the-next-frontier-of-emergency-medicine-house-calls-following-emergency-room-/2024/04#:~:text=The%20new%20program%20is%20called,an%20ED%20to%20Home%20program
- Connolly, L. (2024b, November 27). UC Davis Health brings in-home urgent care to Sacramento. news. https://health.ucdavis.edu/news/headlines/uc-davis-health-brings-in-home-urgent-care-to-sacramento-region/2023/08
- Crowley, C., & Stuck, A. (2016). San Diego; West Health institute. accessed online: https://westhealth.org/wp-content/uploads/2016/04/An-Overview-of-Options-for-Home-based-Healthcare-at-the-Emergency-Department.pdf
- Dispatch Health. (2025). DispatchHealth - urgent care at home. Inova. https://www.inova.org/our-services/dispatchhealth-urgent-care-home
- Emory University. (2023, June 15). DispatchHealth and Emory Healthcare announce collaboration to offer in-home care to patients in Metro Atlanta: Emory University: Atlanta ga. News. https://news.emory.edu/stories/2023/06/hs_ehc_dispatchhealth_collaboration_in_home_care_options_15-06-2023/story.html#:~:text=Since%20the%20company’s%20inception%20in,billion%20in%20medical%20cost%20savings
- Filbin, P. (2023, August 24). Exploring the long-term viability of the SNF-at-home model. Home Health Care News. https://homehealthcarenews.com/2023/08/exploring-the-long-term-viability-of-the-snf-at-home-model/
- Fortune Business Insights. (2025, March 12). U.S. Home Healthcare Services Market Size: Growth [2032]. U.S. Home Healthcare Services Market Size | Growth [2032]. https://www.fortunebusinessinsights.com/u-s-home-healthcare-services-market-105568
- Hospital at Home Users Group. (2020, December 10). Mount Sinai: Hospital-level care for adult patients where they live: Hospital at home. Hospital-level care for adult patients where they live | Hospital at Home. https://www.hahusersgroup.org/sites/mount-sinai/
- Hostetter, M. (2020, July 7). Has the time finally come for hospital at home? | commonwealth fund. Commonwealth Fund. https://www.commonwealthfund.org/publications/2020/jul/has-time-finally-come-hospital-home
- Johns Hopkins Medicine. (2025). Nursing. https://www.hopkinsmedicine.org/care-at-home/care-services/skilled-care/nursing
- Kaiser Permanente. (2025). Home health. Care at Home. https://homecare-scal.kaiserpermanente.org/home-health-2-2/
- Lee Health. (2025). Mobile Urgent Care: Dispatchhealth | lee health. https://www.leehealth.org/our-services/urgent-care/mobile-urgent-care-dispatch-health
- Mashaw, A. (2023, December 19). Advanced care at home at scale in an integrated health care system. AJMC. https://www.ajmc.com/view/advanced-care-at-home-at-scale-in-an-integrated-health-care-system
- Mass General. (2023, September 11). Mass General Brigham’s Home Hospital expands to Brigham and Women’s Faulkner Hospital. Brigham and Women’s Faulkner Hospital. https://www.brighamandwomensfaulkner.org/about-bwfh/news/mass-general-brighams-home-hospital-expands-to-bwfh
- Mayo Clinic. (2025). Home Care Services & Treatment. Mayo Clinic Health System. https://www.mayoclinichealthsystem.org/services-and-treatments/home-care
- Mishra, V., Lloyd, S., & Barron, M. (2024). The State of Health at Home Models. ama-assn. https://www.ama-assn.org/system/files/2019-09/prp-care-delivery-payment-models-2018.pdf
- Noguchi, Y. (2023, April 29). Post-pandemic, even hospital care goes remote. NPR. https://www.npr.org/sections/health-shots/2023/04/29/1167392633/hospital-at-home-remote-care
- Northwell Health. (2025). Northwell Health at Home. https://www.northwell.edu/doctors-and-care/at-home
- Okaka, A. (2024, April 21). How expanded reimbursement for RTM and RPM is changing care. https://www.advisory.com/topics/telehealth/2024/04/expanded-reimbursement-for-rtm-and-rpm
- Pandit, J. A., Pawelek, J. B., Leff, B., & Topol, E. J. (2024, February 27). The hospital at home in the USA: Current status and future prospects. NPJ digital medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC10899639/
- Paulson, M. R., Shulman, E. P., Dunn, A. N., Fazio, J. R., Habermann, E. B., Matcha, G. V., McCoy, R. G., Pagan, R. J., & Maniaci, M. J. (2023, February 9). Implementation of a virtual and in-person hybrid hospital-at-home model in two geographically separate regions utilizing a single command center: A descriptive cohort study. BMC health services research. https://pmc.ncbi.nlm.nih.gov/articles/PMC9911182/
- Penn Medicine. (2021, May 5). New Emergency Department program - penn medicine. New Emergency Department Program - Penn Medicine. https://www.pennmedicine.org/news/news-releases/2021/may/new-emergency-department-program-enables-patients-to-recover-at-home-safely
- Raths, D. (2023, December 18). Is there a ‘snospital-at-home’ program in your health system’s future? | healthcare innovation. hcinnovationgroup.com. https://www.hcinnovationgroup.com/population-health-management/home-based-care/article/53080849/is-there-a-snospital-at-home-program-in-your-health-systems-future
- RUSH.edu. (2021). Rush stories. Rush. https://www.rush.edu/news/rush-and-dispatchhealth-announce-partnership-bring-high-acuity-home-medical-care-Chicago
- Sanford Health. (2025). In-home medical services: Home care. https://www.sanfordhealth.org/medical-services/senior-services/home-care
- Scott, T. (2024, May 15). Sens. Scott, Carper introduce bill to extend the hospital at Home Waiver Program for five years. U.S. Senator Tim Scott of South Carolina. https://www.scott.senate.gov/media-center/press-releases/sens-scott-carper-introduce-bill-to-extend-the-hospital-at-home-waiver-program-for-five-years/#:~:text=WASHINGTON%20%E2%80%94%20Today%2C%20U.S.%20Senators%20Tim,waiver%20program%20for%20five%20years
- Vaidya, A. (2024, May 9). House committee advances Bill Extending Telehealth, hah flexibilities: TechTarget. Virtual Healthcare. https://mhealthintelligence.com/news/house-committee-advances-bill-extending-telehealth-hah-flexibilities
- Vespa, J. (2021, October 8). Demographic turning points for the United States: Population projections for 2020 to 2060. Census.gov. https://www.census.gov/library/publications/2020/demo/p25-1144.html
- Zorn, A. (2021, August 4). SNF-at-home model becoming “critical player” for success. Skilled Nursing News. https://skillednursingnews.com/2021/08/snf-at-home-model-becoming-critical-player-for-success/
.png?width=125&height=125&name=logo_wt%20(3).png)





.png?width=300&name=CancerX%20Decimal%20Banner%20(2).png)